Project Description
Hospitals Urgently Need Circular Economy Solutions

Commercial reprocessing companies clean, inspect and repair SUDs before they test, disinfect/sterilize, package, and ship the product.
By reprocessing “single-use” medical devices (SUDs), hospitals reduce costs, waste, and greenhouse gas emissions. They also build a more resilient supply chain by keeping devices in circulation longer, reducing the demands of the global supply chain. At a time when U.S. hospitals are expected to lose $54B, circular economy solutions are desperately needed (Kaufman, Hall and Associates, 2021).
Outside healthcare, the “Right to Repair” movement is enabling consumers to extend the life of other products, including mobile phones or tractors, demonstrating how circular economy solutions across industries play an important role in enhancing financial and environmental sustainability.
Maximizing Value of Healthcare Products
The market for reprocessed medical devices is growing rapidly as market forces – including supply chain disruptions, skyrocketing costs, and climate change concerns – force hospitals to adopt more circular programs to address these challenges.
There’s room for significant growth. AMDR estimates that if all U.S. hospitals reprocess SUDs at the rate of the top performing hospitals, over $2.2 billion would be saved – per year!
In healthcare, however, reprocessing of SUDs is an exception to the rule: Many instruments and pieces of equipment are purchased and used without the healthcare consumer being able to repair and reuse in order to reduce costs and environmental harm. Reusing what you have, medical equipment is central to minimizing needless consumption and waste, not to mention lowering costs and emissions. Hospitals and surgical centers reuse a range of medical equipment in different ways:
Sterile Processing Department (SPD) for reusable products. Also known as Central Sterile or Sterile Processing Departments (SPD), these in-house reprocessing programs have been used to decontaminate, clean, and sterilize medical devices since at least 1928 when the practice was first moved out of the surgical suite (Steris Healthcare). SPDs range from large, complex production environments that reprocess hundreds of instrument sets and devices to small facilities dedicated to a specific department or specialty care area that reprocess a limited variety and volume of instruments (Health Facilities Management Magazine, April 2019). Equipment sent to SPD range from scissors to wheelchairs.
 Commercial repair and/or sterilization for reusable products. When reusable equipment needs repair, hospitals frequently partner with vendors who repair the products to bring them to safe standards. These companies may also provide cleaning and disinfecting of reusable hospital equipment, or hospitals may send used equipment directly to companies that provide this service. Often, these services are used by hospitals that either don’t have an in-house SPD or are too complex to process and repair internally. Endoscopes, for example, are reusable devices frequently sent to third-party repair companies. However, the principle behind “Right to Repair” is frequently challenged in this effort to maximize the life of medical equipment, through restrictive contracts or de-facto monopolization of equipment maintenance. Unlike SUD reprocessing, the right to repair has not been codified in healthcare instrument or asset acquisitions.
Commercial repair and/or sterilization for reusable products. When reusable equipment needs repair, hospitals frequently partner with vendors who repair the products to bring them to safe standards. These companies may also provide cleaning and disinfecting of reusable hospital equipment, or hospitals may send used equipment directly to companies that provide this service. Often, these services are used by hospitals that either don’t have an in-house SPD or are too complex to process and repair internally. Endoscopes, for example, are reusable devices frequently sent to third-party repair companies. However, the principle behind “Right to Repair” is frequently challenged in this effort to maximize the life of medical equipment, through restrictive contracts or de-facto monopolization of equipment maintenance. Unlike SUD reprocessing, the right to repair has not been codified in healthcare instrument or asset acquisitions.
Commercial reprocessing for SUDs. The U.S. Food and Drug Administration (FDA) created a regulatory pathway over 20 years ago for SUDs to ensure reprocessed SUDs are safe and effective. Europe, as of 2017, has a similar, manufacturer level of regulatory oversight of SUD reprocessing. Today, over 300 types of SUDs have been cleared by regulatory authorities for reprocessing by commercial entities, finding they are “substantially equivalent” to the original device. Nearly 12,000 hospitals and surgical centers in the U.S. and Europe partner with commercial reprocessors to reduce costs, build supply chain resilience, and reduce greenhouse gas emissions.
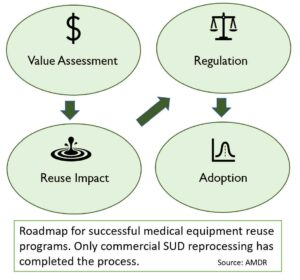
 Commercial SUD reprocessors may be independent of the original equipment manufacturer (OEM), a subsidiary of the OEM, or may have a collaborative relationship with the OEM. Unlike other types of medical device/equipment repair or reuse, commercial SUD reprocessing is highly regulated and the right of hospitals to reprocess their SUDs is firmly established in law and regulation. The successful history of SUD reprocessing validates the effectiveness of reuse as a core function in healthcare to extend product life and incur the ancillary benefits associated with doing so. Members of the Association of Medical Device Reprocessors (AMDR) have demonstrated there is a safe, successful, and circular business model in SUD reprocessing.
Commercial SUD reprocessors may be independent of the original equipment manufacturer (OEM), a subsidiary of the OEM, or may have a collaborative relationship with the OEM. Unlike other types of medical device/equipment repair or reuse, commercial SUD reprocessing is highly regulated and the right of hospitals to reprocess their SUDs is firmly established in law and regulation. The successful history of SUD reprocessing validates the effectiveness of reuse as a core function in healthcare to extend product life and incur the ancillary benefits associated with doing so. Members of the Association of Medical Device Reprocessors (AMDR) have demonstrated there is a safe, successful, and circular business model in SUD reprocessing.
The Right to Reprocess
Consistent with our mission, AMDR stands in support with our hospital and surgical center partners in viewing all medical equipment as assets that healthcare facilities – the consumers of these items – have a right to repair or reprocess.
The larger right to repair movement gaining attention in Congress, state legislatures, and in regulatory agencies underscores the rights consumers have to repair the products they buy, including the rights to choose service or repair providers not affiliated with the original manufacturer. When it comes to medical equipment, hospitals are just like any other consumers of products.
Many electronics consumers are experienced in planned obsolescence measures some manufacturers build into mobile phones, MP3 players, and earbuds. The same is true for hospitals and surgical centers that often have little option but to accept the latest model equipment from device manufacturers, which may mean accepting devices with wasteful, built-in planned obsolescence.
In the face of this, SUD reprocessing can serve as a model for how the “right to repair” principles can be exercised elsewhere in healthcare. Establishing a regulatory framework around the repair and maintenance activities, creating transparency around the impact (financial and environmental) of unrestricted (but regulated) reuse and repair, and establishing firmly the safety and reliability of reused equipment are among the elements in this.
“Right to Repair” Challenges in SUD Reprocessing
Despite the fact that use of reprocessed SUDs requires FDA or other agency clearance or approval, and that it is a well-established practice at over 9,400 hospitals worldwide, some OEMs are routinely seeking to infringe on this right to repair.
AMDR urges hospitals and surgical centers to partner with medical device makers and reprocessors that seek to maximize the value of device assets (extend their life) and therefore reduce costs, waste, and emissions. Efforts that inhibit a hospital’s right to reprocessing and undermine reprocessing programs include:
- OEM Staff Influence: When some OEMs lend staff to the operating room, hospitals may become overly reliant on that staff and it may amount to greater costs and consumption by the hospital. AMDR is aware of some OEMs, once entrenched, who threaten to pull the staff unless the hospital agrees to stop reprocessing some SUDs. AMDR urges hospitals and surgical centers to only work with vendors supportive of reprocessing programs.
- Software “upgrades:” Another threat to the rights of hospitals to reprocess SUDs is some OEM use of software “updates” or “upgrades” that prevent reprocessed versions of these devices from working with consoles or generators. By manufacturing the devices with microchips and updating the software on the generators, some OEMs are causing more waste, cutting out competition, and increasing a hospital’s reliance on the OEM by preventing reprocessed versions of medical devices from working. AMDR urges hospitals and surgical centers to work with vendors that do NOT restrict the facility’s ability to reprocess and strongly counter such measures (such as refusing software “updates”) when they encounter them as antithetical to the interests of the health institution.
- Forced obsolescence: The use of “erasable programmable read-only memory” (EPROM) chips and “Radio Frequency Identification” (RFID) tags in the handles of surgical and diagnostic medical devices are being used to intentionally limit the use of the device more than once. Employed based on unsupported “patient safety” claims, these chips are inserted to prevent additional device uses after a single use. AMDR has evidence that an OEM with its own reprocessing division (not an AMDR member), includes such chips, not just to discourage reprocessing, but to discourage reprocessing with competing vendors. Further, billed as “innovation,” some medical device manufacturers introduce new models of existing technology that are designed to make it impossible to reprocess and reuse them. When such generational innovation disallows reprocessing, the hospital loses the savings and environmental benefits due to the OEM’s locking out reprocessing. While many technology innovations come with clinical and technological advantages to prior models, the launch of devices with reprocessing “kill switches” or “locks” – without scientifically backed clinical advantages – is becoming more and more common. AMDR encourages hospitals and surgical centers to inform these companies they wish such activity to stop, to resist new makes and new models with such “kill chips,” and to reward companies that support reprocessing.
- Voiding Warranties. AMDR is aware of some OEM contracts that include provisions to void warranties on equipment used in conjunction with reprocessed devices. We are also aware of OEM sales representatives threatening to void those warranties for the same reason. AMDR does not believe these companies can lawfully refuse warranty support of generators and consoles, though they are not required to provide warranty for reprocessed products. AMDR urges hospitals and surgical centers to resist these threats and instead reward companies that promote reprocessing.
AMDR has a resource page that further addresses each of these topics. If you are experiencing an OEM that has created obstacles to reprocessing, let us know. We’ll keep your information confidential. Describe the issue in an e-mail to info@AMDR.org.

