“Medical device reprocessing? Is that safe?”
If you have a role in patient care, this might have been your first thought when you heard about single use device (SUD) reprocessing. With “do no harm” as your oath, you want to be sure that your patients are safe, and you might be hesitant to trust reprocessed devices.
Patient safety is at the center of AMDR’s mission. We encourage clinicians, regulators, and procurement leaders to do their due diligence to explore the evidence about whether reprocessed devices are safe.
After decades of research, government oversight, and successful clinical practice around the world, that evidence is clear: regulated reprocessed SUDs are safe and effective.
Regulated Devices Are Safe Devices
Regulation makes modern medicine possible. On the basis of strict scientific review and oversight, regulators determine whether devices and pharmaceuticals are safe and effective.
Strong regulations have ensured the safe use of reprocessed SUDs in thousands of hospitals across four continents. Reprocessing is a case study in science-based regulation.
Here’s how it works:
Our industry welcomes oversight.
25 years ago, industry leaders established AMDR to advocate for a fair market and strict regulatory oversight. AMDR’s testimony to Congress (pp. 128-135) helped secure the regulatory framework that has worked ever since.
Today, regulation remains key to our policy agenda, while nearly half of our Code of Conduct is devoted to ensuring regulatory compliance by our member companies.
We emphasize strong regulation because it is the best way to protect patient safety—and thus the legitimacy of our industry.
Reprocessing companies must prove that their products meet or exceed the same safety and performance requirements as their original counterparts.
Even at the maximum number of reprocessing cycles, the device must remain substantially equivalent to the original in its cleanliness, sterility, and performance.
Reprocessing companies are considered “manufacturers” and must likewise adhere to identical standards and expectations as original manufacturers.
Regulations require extensive validation data to ensure reprocessed products are safe and effective before they go to market.
Regulators look at everything, from the number of times or “cycles” a device can be reprocessed to whether the sterilization methods degrade sensitive components.
Even logistical questions—such as the time and temperature at which used devices are stored before reprocessing—are put under the microscope as they are relevant to ensuring device cleanliness, sterility and performance.
Reprocessing is a benchmark for rigorous scientific review.
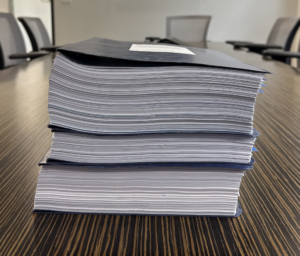 At left: This is a 510(k) submission for a reprocessed device. Its size illustrates the depth of testing and documentation provided for FDA review.
At left: This is a 510(k) submission for a reprocessed device. Its size illustrates the depth of testing and documentation provided for FDA review.
510(k) review is the FDA’s premarket clearance pathway, where a manufacturer or reprocessor must demonstrate that their device is substantially equivalent to another legally marketed device in its intended use, safety, and performance. If the FDA agrees, the device is cleared for marketing.
With some differences in terminology, most reprocessing regulations follow the above framework, including:
![]() the Medical Device User Fee and Modernization Act in the United States;
the Medical Device User Fee and Modernization Act in the United States;
![]() the Medical Device Regulation in the European Union;
the Medical Device Regulation in the European Union;
![]() the official position of the United Kingdom; and
the official position of the United Kingdom; and
![]() the approaches of many other countries around the world.
the approaches of many other countries around the world.
AMDR maintains an updated compendium of global reprocessing regulations and standards. Please click here to receive it.
Sometimes, particularly in jurisdictions that lack strong regulations and commercial reprocessing industries, medical devices are sterilized and reused in-house within health systems.
While sometimes referred to as “reprocessing,” the safety and quality of these devices cannot be guaranteed due to lack of oversight. AMDR discourages this practice.
Instead, we support developing regulatory frameworks in countries that lack them, growing the commercial reprocessing industry, and supporting innovation in SUD design to expand the list of devices approved for reprocessing.
But aren’t these devices labeled for “single-use” only?
According to the U.S. FDA, the “single-use” label does not mean a device cannot be safely reprocessed. Rather, it often means the original manufacturer simply decided not to do the necessary testing to prove that it can be.
Additionally, reprocessed devices are still “single-use.” They are not simply “reused” between patients, but must be rigorously cleaned, sterilized, inspected, function-tested, and repackaged before each reprocessing cycle.
What Does the Science Say?
Extensive government data and independent, peer-reviewed research have overwhelmingly found that regulated reprocessed devices are as safe and effective as their original counterparts.
 The U.S. Government Accountability Office (GAO) is an independent federal agency that provides auditing and research services for the government. In a major 2008 report, the GAO found that reprocessed devices do not pose a greater safety risk than original devices.
The U.S. Government Accountability Office (GAO) is an independent federal agency that provides auditing and research services for the government. In a major 2008 report, the GAO found that reprocessed devices do not pose a greater safety risk than original devices.
This extensive review included:
- FDA data on reprocessing, hospital infections, and device-related adverse events;
- studies published in peer-reviewed journals; and
- interviews with FDA officials, clinicians, device manufacturers, and reprocessors.
Already in 2000, as the FDA prepared its first reprocessing regulations, the GAO reported that little available evidence indicated any increased risk to patients from SUD reprocessing. The 2008 report leaned on eight years of data and research that had emerged since—covering thousands of hospitals and hundreds of thousands of reports.
As such, the 2008 GAO report is one of the most important resources on reprocessing safety to date.
AMDR has highlighted the linked reports for readability.
 AMDR’s bibliography of peer-reviewed research and other scientific literature on reprocessing includes more than two-dozen articles about safety. This body of research represents the overwhelming scientific opinion that reprocessed devices are safe.
AMDR’s bibliography of peer-reviewed research and other scientific literature on reprocessing includes more than two-dozen articles about safety. This body of research represents the overwhelming scientific opinion that reprocessed devices are safe.
 A 2015 study compared the defect rates between reprocessed and original versions of a particular device.
A 2015 study compared the defect rates between reprocessed and original versions of a particular device.
Evaluating more than 3,100 devices over a seven-month period, the study found that reprocessed devices actually have a significantly lower rate of defects than originals.
While more research is needed to determine whether and why this is generally true, reprocessors have to prove that their devices can be safely used after every single reprocessing cycle. Additionally, while original equipment manufacturers only have to “batch test” their products, reprocessors must test and inspect 100 percent of their devices.
We speculate that, as a result of this highly rigorous process, reprocessors might catch defects sooner and more reliably than original equipment manufacturers.
Reprocessing Reduces Harm
The science makes clear that reprocessed SUDs are not more likely to harm patients.
We argue that by reducing carbon emissions, soaring device costs, dangerous pollution, and critical vulnerabilities in healthcare supply chains, reprocessing actually reduces harm.
The global health sector accounts for almost 5% of all greenhouse gas emissions. Clinicians cannot make good on the Hippocratic Oath if their practices are a leading cause of climate change.
This article explores why healthcare professionals have a moral imperative to reduce emissions, and why leading institutions are endorsing reprocessing as a solution.
 Hospitals are running out of money, and often cutting back on patient care as a result. Meanwhile, many people avoid treatment because they cannot afford it.
Hospitals are running out of money, and often cutting back on patient care as a result. Meanwhile, many people avoid treatment because they cannot afford it.
Reprocessing saves money, and saving money could mean saving or improving lives.
 Research has found that when hospitals incinerate medical waste, it generates dangerous air pollution that harms patient populations—particularly the most vulnerable.
Research has found that when hospitals incinerate medical waste, it generates dangerous air pollution that harms patient populations—particularly the most vulnerable.
Healthcare waste shouldn’t harm patients. By reducing the number of devices sent to the incinerator, reprocessing helps fulfill our obligation to “do no harm.”
 During the pandemic, shortages of critical medical supplies upended healthcare around the world. Ongoing trade and other geopolitical tensions compound this threat.
During the pandemic, shortages of critical medical supplies upended healthcare around the world. Ongoing trade and other geopolitical tensions compound this threat.
Reprocessing protects healthcare supply chains by reducing reliance on imported devices and materials. The next disruption will be just as hard, but reprocessing can help us be more resilient.
A Note on Misinformation
The above information is based on peer-reviewed science, government reports, and/or other third-party sources.
However, some medical device manufacturers view reprocessing as a threat to their business models, and try to undermine reprocessing by promoting misinformation about the safety of reprocessed devices.
Please see our page about anti-reprocessing interference to learn more about this issue, and our Action Alerts and Technical Tips for guidance about specific misleading claims.


